Bodywork support for survivors of severe TBI in the chronic phase of their recovery.
Traumatic Brain Injury - the new silent epidemic continues to be on the rise in 204 countries.(https://pmc.ncbi.nlm.nih.gov/articles/PMC12034675/ )
TOUCH has never felt more necessary
TBI survivors with their nurse and PT, at Shepherd Rehabilitation Center, Atlanta GA, 2022
For the last 20 years advancement in neurosurgical approaches made saving human brains possible.
Although they potentially decrease mortality for severe TBI cases, survivors are left with life-long sequele of cognitive, physical and psychological symptoms.
Mood, anxiety, and substance use disorders were most prevalent disorders across five years of follow-up post-injury, with a steady decline in prevalence over time( according to DSM-IV Axis I).
The crude categorization of TBI on mild, moderate and severe and the believe that a mild injury will produce mild clinical picture have been a problem for years, and are often not reflective of a patient’s long-term recovery.
The new approach to classifying TBI is based on The CBI-M Pillars. CBI-M consists of four pillars: clinical, biomarker, imaging, and modifiers.https://www.ninds.nih.gov/news-events/directors-messages/all-directors-messages/new-framework-classifying-traumatic-brain-injury-tbi-could-transform-patient-care
A mild injury does not necessarily mean a mild outcome. As high as 75% of the people looking for mental health and substance use treatment also have a brain injury. ( Brain links ) https://www.tndisability.org/tennessee-brighter-futures
The current rehabilitation and treatment programs provide limited options for improving the survivors’ QOL.
Most of TBI survivors has developed symptoms of PTSD, regardless of the degree(or absence) of their physical impairment..
The extent to which a person with TBI needs to reconstruct the trauma narrative to recover from PTSD has yet to be empirically determined. Several large-scale studies have reported that mild to severe TBI are associated with increased risk for PTSD.https://pmc.ncbi.nlm.nih.gov/articles/PMC3182010/One possibility for this observation may be that people who sustain a M or S TBI do not have a coherent narrative of their traumatic experience because of the impaired consciousness secondary to the brain injury, and this may impede their capacity to contextualize the experience in their autobiographical memory base.
Recent studies suggest that after TBI the treatment of choice for PTSD should not involve trauma focused exposure therapy. This treatment is based on extinction learning, which occurs when a conditioned stimulus is repeatedly administered with a frequent adverse effect - re-traumatization.
There is a tremendous need for development of therapies with a direct ability to improve function in the post-TBI existence.
This story is an insight of a single clinician with experience of >27 years working with ANS of diverse TBI patient populations, in different clinical settings ( ICU 2 cases, Shepherd center -17 cases, out-of -hospital settings -7 cases)
It illustrates the use of Manual therapy techniques -VM( Visceral Manipulations), Neuro- meningeal manipulations, LDT ( Lymph Drainage Therapy) and CST - applied to Vagus Nerve and its outputs with focus on training Autonomic Nervous System (ANS ) flexibility and stability.
The most important fact is that the clinician should remain in constant presence for the emerging changes in the patient’s autonomic state and adopt its approach to assure their sense of safety.
I wish I could say these are techniques only ... but i can’t ...It’s a constant exchange of information between the clinician and the tissues through infinite interoceptive, proprioceptive, vestibular and peri- personal perceptual inputs.
Each of these precise Manual techniques I chose bellow to illustrate potential use for survivors of TBI were carefully chosen and applied, at each session, depending on the prevalent symptoms and particularly on each patient’s autonomic state.
For example, mobilizing Vagus nerve through the palate and pharynx is worth trying at any moments you notice clenching teeth, frequent swallowing, fast breathing cycles or arterial pulse, when these symptoms are result of constant firing of impulses between these nerves and their nuclea in the brain.
*Index intraorally mostly on the hard palate contacting a little bit the soft palate)
* other hand engaging hyoid bone in a caudal movement
Mobilizing Vagus nerve through tensor Velli palatini muscle (making it unique as the only soft palate muscle not controlled by the vagus nerve (CN X) and pharynx (Salpingo-pharyngeal muscle)assisting in swallowing and opening the Eustachian tube( innervated by pharyngeal branches of Vagus n.)
It may seem or we may think that it is easy to access Vagus N in the neck . According to Jean-Pierre Barral” It’s not easy to palpate Vagus n in the neck. We may not be able to “palpate it directly” but there are various locations we can access it in the neck- via the Superior Laringeal nerve, the Recurrent Laringeal, or the Auricular branch at the External Ear canal”( J.P.Barral, Alain Grobier, Visceral -Vascular Manipulations, 2025)
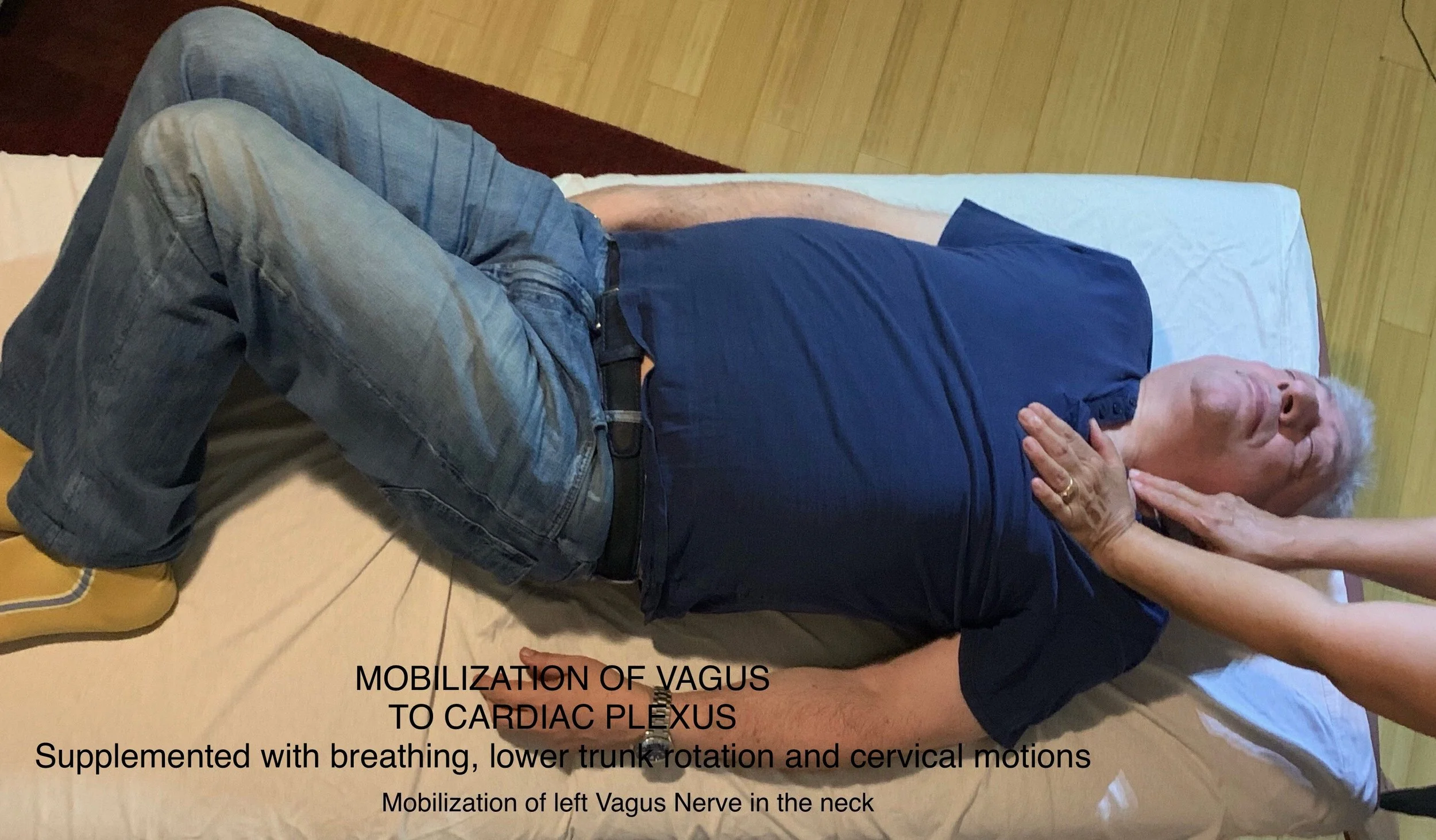
Mobilization of Vagus n in the neck to the Cardiac plexus
That’s how mobilizing of the Vagus N to the Cardiac Plexus may look, synchronized with patients breathing cycle and facilitated by lower body and head rotation ( for fascia pull) to opposite side.
This leads us to the reality fact-check that due to the proximity these fine structures are situated in the neck, the manual access to them is inadvertently affecting both - the Vagus n. and the Sympathetic chain. In which case we are talking about Vago-sympathetic mobilization. As JP Barral advises, “The main thing is to focus on feeling the precise micro-zone of neural fixation, and NOT TO DECIDEFOR OUSELVES the outcome of the technique. The organism CAN SELF-REGULATE, as long as the manipulation is subtle, precise and not painful”. A clever approach is offered by Physical Medicine devices, combining manual access with static electricity :
Stimulation of Vagus N and Sympathetic chain in the neck (bilaterally or unilaterally, according to symptoms and present autonomic state ) using static electricity through HIVAMAT device
There are many more “ manual/bodywork techniques” that we need to revise, may be in a second part of this topic blog. Such as:
Vagus nerve manipulation at gastro-esophageal sphincter.
Elongation of all branches of subdiaphragmatic Vagus - through Mobilization of Mesentery.
MLD(manual lymph drainage ) of head and Brain for facilitating interstitial fluid (ISF ) flow through glymphatic system.
Integration of ANS through CAN- Central Autonomic Nerve - Particularly important for the post TBI conditions
It is imperative to stress the importance of some Myths, Realities and Evidence for solutions , when working with ANS ( most phenomena are happening inadvertently, at each encounter with any patient. Even during coma or other states of impaired consciousness!).
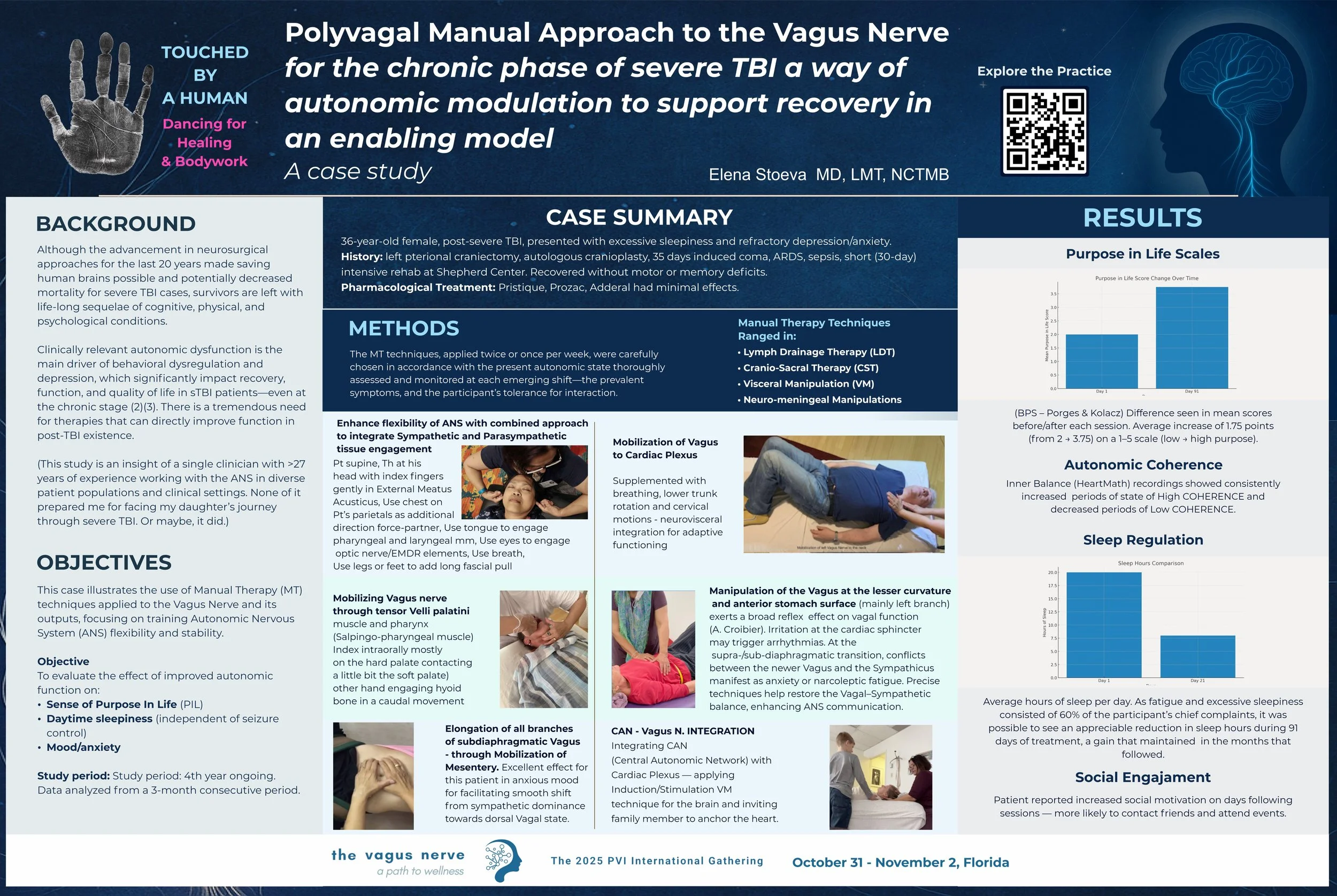
This case study illustrates the use of Manual therapy techniques -VM( Visceral Manipulations), Neuro- meningeal manipulations, LDT ( Lymph Drainage Therapy) and CST(Cranio-sacral therapy) - for Improving QOL(Quality Of Life) of survivors of sTBI expressed by strengthen sense of agency, decreased daytime sleepiness(independent from seizure control) and elevated mood:
The study is in its 4th year, monitored by PURPOSE IN LIFE SCALES per BPS(Porges and Kolacz) and HRV by HeartMath Inner Balance. It was presented at the PVI ( https://www.polyvagalinstitute.org )conference 2025, Amelia Island, FL.
Read the abstract here: https://docs.google.com/document/d/1-EPlBLWUU3bdqmX4nevOwJBu8W8njfeh/edit?usp=drivesdk&ouid=114896352605034801517&rtpof=true&sd=true
The results were strikingly conclusive of:
CONCLUSION/DISCUSSION : 21 sessions of specific CST/VM/NM/MLD therapy resulted in measurable improvement of the flexibility of her ANS, statistically enhanced purpose in life and functionally optimized ratio of sleep/wake hours.
If this case demonstrates the potential for improvement of the sense of purpose and changing the impaired sleeping patterns - from excessive sleepiness to mobilization and activities during the day, as a result of Manual th techniques, then a larger study would be proving the value of this approach in the rehabilitation of post sTBI conditions.
Recognition of this approach is critical to institution of appropriate therapy for relieving the challenging existence of survivors of TBI.
That’s why we should never stop searching for ways to support this amazing tissue The BRAIN and the whole HUMAN BEING that it belongs to.
🧠♥️🧠♥️
——————————————————————————-
REFERENCE:
Williamson JB, Heilman KM, Porges EC, Lamb DG, Porges SW. A possible mechanism for PTSD symptoms in patients with traumatic brain injury: central autonomic network disruption. Front Neuroeng. 2013 Dec 19;6:13. doi: 10.3389/fneng.2013.00013. PMID: 24391583; PMCID: PMC3867662.
Howlett JR, Nelson LD, Stein MB. Mental Health Consequences of Traumatic Brain Injury. Biol Psychiatry. 2022 Mar 1;91(5):413-420. doi: 10.1016/j.biopsych.2021.09.024. Epub 2021 Oct 2. PMID: 34893317; PMCID: PMC8849136.
LM Li, Ekawat Vichayanrat, Martina del Giovane, Helen Hoi Lun Lai, Valeria Iodice - Autonomic dysfunction after moderate-to-severe traumatic brain injury: symptom spectrum and clinical testing outcomes: BMJ Neurology Open 2022;4:e000308.
Esterov D, Greenwald BD. Autonomic Dysfunction after Mild Traumatic Brain Injury. Brain Sci. 2017 Aug 11;7(8):100. doi: 10.3390/brainsci7080100. PMID: 28800081; PMCID: PMC5575620.
Friedman BH. An autonomic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biol Psychol. 2007 Feb;74(2):185-99. doi: 10.1016/j.biopsycho.2005.08.009. Epub 2006 Oct 27. PMID: 17069959.
Kolacz J, Kovacic KK, Porges SW. Traumatic stress and the autonomic brain-gut connection in development: Polyvagal Theory as an integrative framework for psychosocial and gastrointestinal pathology. Dev Psychobiol. 2019 Jul;61(5):796-809. doi: 10.1002/dev.21852. Epub 2019 Apr 5. PMID: 30953358.
Postconcussive Sleep Problems and Glymphatic Dysfunction Predict Persistent Working Memory DeclineYi-Tien Li, David Yen-Ting Chen, Duen-Pang Kuo, Yung-Chieh Chen, Sho-Jen Cheng, Li-Chun Hsieh, Yung-Hsiao Chiang, and Cheng-Yu Chen Journal of Neurotrauma 0 0:0
CranioSacral Therapy and Visceral Manipulation: A New Treatment Intervention for Concussion RecoveryGail Wetzler, Melinda Roland, Sally Fryer-Dietz, and Dee Dettmann-AhernMedical Acupuncture 2017 29:4, 239-248
Liem, Torsten and Neuhuber, Winfried. "Osteopathic Treatment Approach to Psychoemotional Trauma by Means of Bifocal Integration" Journal of Osteopathic Medicine, vol. 120, no. 3, 2020, pp. 180-189. https://doi.org/10.7556/jaoa.2020.021
Kearney BE, Corrigan FM, Frewen PA, Nevill S, Harricharan S, Andrews K, Jetly R, McKinnon MC, Lanius RA. A randomized controlled trial of Deep Brain Reorienting: a neuroscientifically guided treatment for post-traumatic stress disorder. Eur J Psychotraumatol. 2023;14(2):2240691. doi: 10.1080/20008066.2023.2240691. PMID: 37581275; PMCID: PMC10431732.
Barral, J.-P. (2022). Manual Therapy Approach to the Brain - Volume 1.
Éric Marlien (2021). New Approach to the Vagus Nerve and the Autonomic Nervous System.
Marlien, E. (2024). De l’homme-animal à l’homme divin. Publishroom.